You Operate. We Recover.
Successes
Real Claims. Real Data
Patients are your business. Maximizing out-of-network reimbursements is ours.
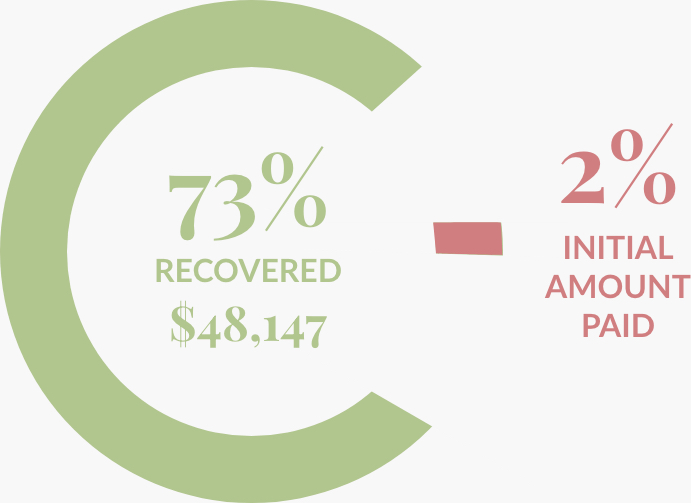
Plastic Reconstructive Surgery
Breast Reconstruction
$66,124 Billed
$1,253 Initial Payment
$48,147 Recovered Dollar Amount
Timeline:

Results:
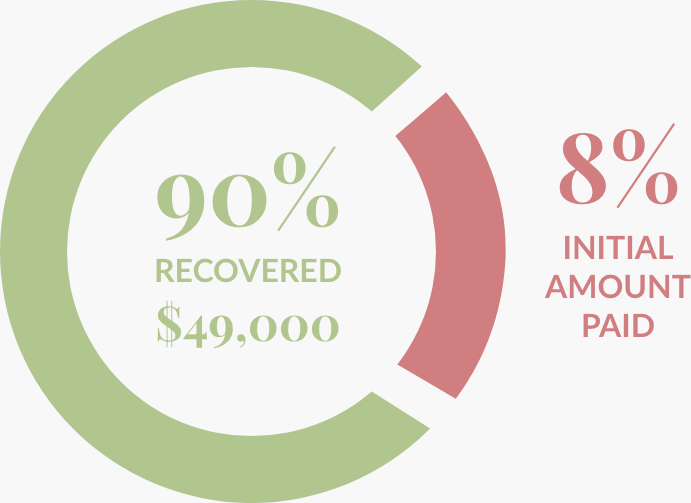
Neurological Surgery
Brain Mass
$54,700 Billed
$4,560 Initial Payment
$49,000 Recovered Dollar Amount
Timeline:

Results:
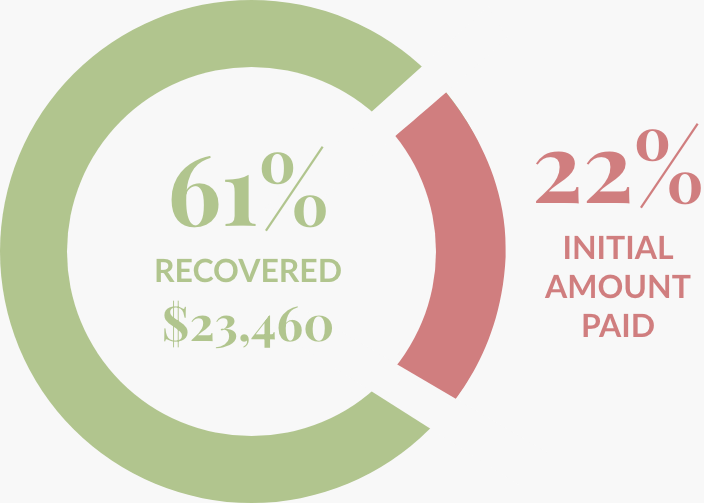
Orthopaedic Surgery
Spine
$38,535 Billed
$8,540 Initial Payment
$23,460 Recovered Dollar Amount
Timeline:

Results: